gastroenterology
The American College of Gastroenterology (ACG) 2010 Annual Meeting
Persistence and Adherence to 5-ASA Therapy for UC in Canada: Relevant Data from the Real-world Setting
San Antonio – New claims data in Canada have revealed that adherence to 5-aminosalicylic acid (5-ASA) among patients with ulcerative colitis (UC) differs significantly among available formulations. These data have important public health implications because adherence to therapy is the single most important defense against relapse and complications of UC. Moreover, less well tolerated and generally more expensive immunomodulators and biologics follow in patients not controlled on 5-ASA, which is the guideline-defined first-line treatment for mild-to-moderate UC. Although multicentre trials with some of the available delayed-release 5-ASA agents have demonstrated that this form of therapy is effective for both acute healing and maintenance, this is clearly dependent on adequate adherence. The Canadian data suggest that high rates of avoidable relapses, incurring increased rates of hospitalization, surgery, and other adverse outcomes that raise cost of care, are being generated by suboptimal rates of 5-ASA adherence overall.
Real-world Data Suggest Need for Increased Adherence
While the data suggest that the specific 5-ASA agent matters in a real-world setting of adherence, there is a need for new strategies to improve adherence.
In an analysis of adherence rates over six months from a database with prescription capture from 10 million people, a steep and steady decline of those who remained on therapy was observed over the course of the study in all five of the 5-aminosalicylic acid (5-ASA) preparations evaluated. However, when the agents were compared, the rates of decline were slower on the once-daily medication with the least pill burden, producing significant differences over the course of six months. For the best performing agent, this included more than double the likelihood of remaining on therapy at six months relative to the worse performing agent. While the data suggest that the specific 5-ASA agent matters in a real-world setting of adherence, the need for new strategies to improve adherence across treatments was another important message discussed at this year’s ACG meeting.
Study Shows Persistence and Adherence Differences between 5-ASA Agents
In this study, a Canadian drug plan database with 83 million entries was searched for new prescriptions of a 5-ASA agent (naive patients or no 5-ASA prescription within the previous six months). Adherence was then tracked at 15-day intervals over six months. Adherence was compared for five 5-ASA formulations or doses. There was data captured on 15,545 patients of whom the mean age was 43.6 years. There were slightly more females than males, but the distribution of both gender and age were similar across the 5-ASA agents assessed. The similarity of treatment groups is important because of the unequal decline in adherence among agents.
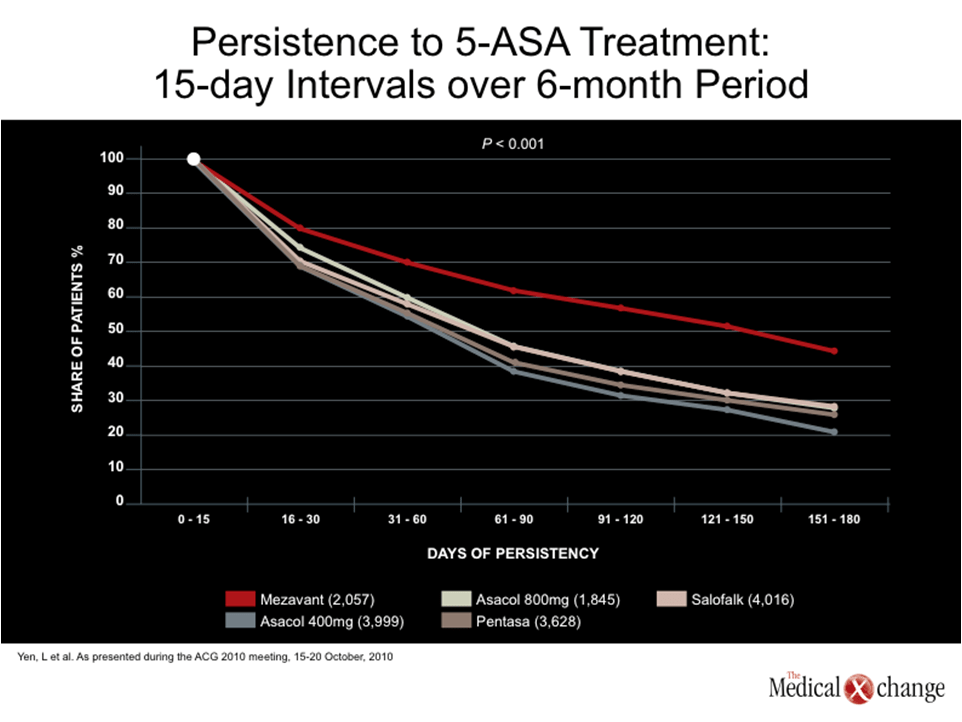
In fact, the curves tracking adherence began to separate at the first 15-day interval. While three of the agents tracked together, Multi-Matrix System (MMX) mesalamine, which offers the simplest dosing scheme among these agents, had already produced a visible advantage in adherence on graphed rates, and this grew progressively over the course of the study (Fig. 1).
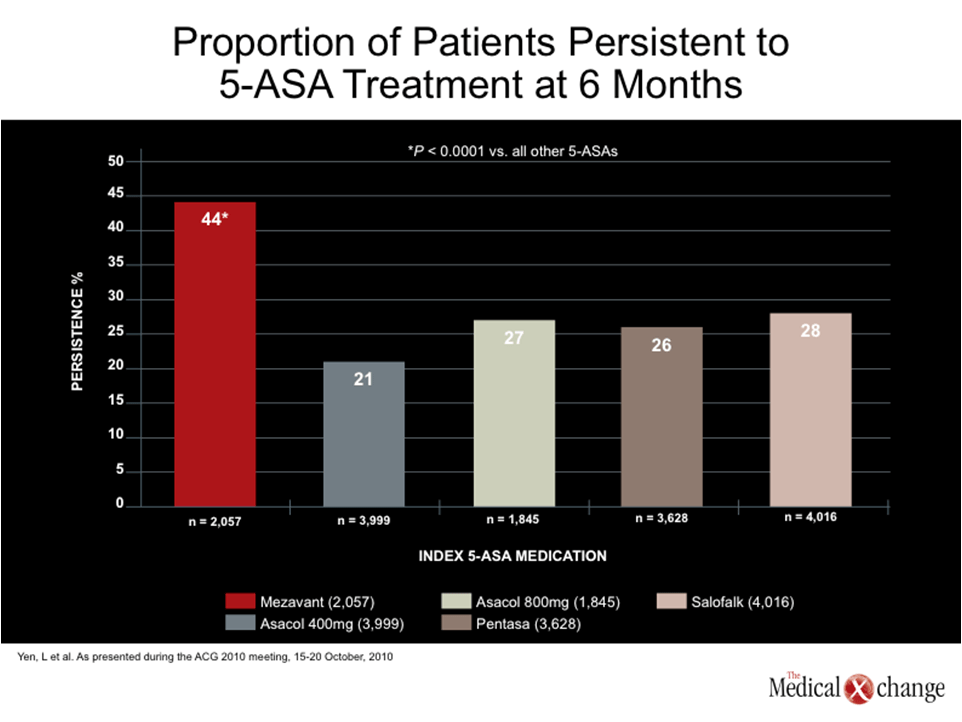
The percentage of patients who remained on therapy at the end of six months was 44% for MMX mesalamine, and a range of 21% to 28% for the other 5-ASA formulations. The advantage of MMX mesalamine was statistically significant (P‹0.0001 for all comparisons) (Fig. 2).
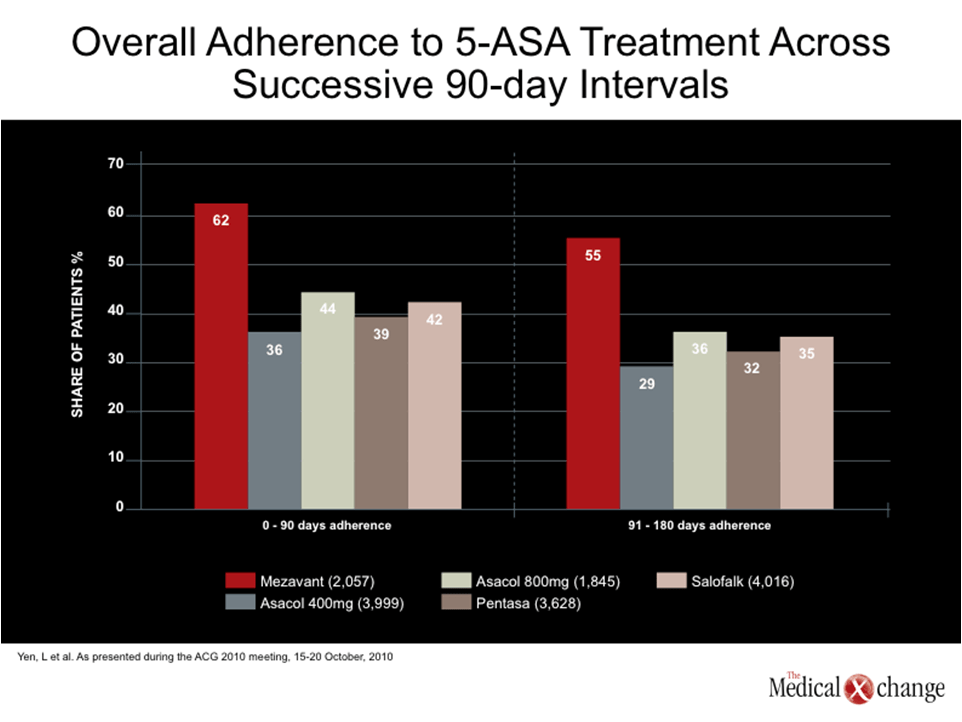
“Patients who were initiated on MMX mesalamine were significantly more persistent, continued treatment after the initial claim, and maintained adherence >80% and >90% more than other 5-ASA products in this analysis,” according to a team of investigators, led by senior author Dr. Subrata Ghosh, Head, Division of Gastroenterology, University of Calgary, Alberta. Further, the percentage of patients adherent to 5-ASA treatment measured across successive 90-day intervals for the entire sample was consistently higher in the MMX group (Fig. 3).
There are two important messages from this study. The first is that simplicity of dosing makes a key difference for adherence in a real-world setting outside of a clinical trial. However, the other message is that adherence rates are suboptimal even on the agent that performed best. The fact that less than half of patients remained on therapy with any agent has important implications for patient outcome and cost of care based on data linking ulcerative colitis (UC) therapy adherence to better outcomes.
Improving upon Adherence to Reduce UC Relapse
Indeed, substantial improvements in adherence “could lead to reduced UC relapse and thus help reduce the economic burden of this chronic disease,” according to Dr. Ghosh and his co-investigators. Importantly, the cost incurred by hospitalizations and complications from non-adherence is not the only issue. The burden of repeated relapses for the patient is considerable. Moreover, patients who fail 5-ASA are placed on immunomodulators or biologics which are not only more expensive, but introduce potential safety issues.
The relative efficacy of 5-ASA formulations has not been well studied, but there is evidence that differences of 5-ASA exposure at the site of inflammation, which is almost certainly dependent on the adequacy of the specific delayed release mechanism, do influence likelihood of healing, a key endpoint in acute treatment, and the likelihood of preventing relapse. Healing, followed by high rates of persistent remission at 12 months, has been demonstrated in large multicentre studies with MMX (Kamm MA et al. Gastroenterology 2007;132:66-75) but translating this into routine clinical care may be different outside of a trial that employs regular follow-up and encouragement for adherence.
Adhering to Treatment and Quality of Life
Poor adherence is hardly unique to the treatment of UC, but the consequences are particularly severe for chronic condition with the potential to progress.
Although simple regimens with low pill burdens are key aspects that may improve patient adherence, the data also suggest that better patient education is needed to help patients link lack of adherence with increased risk of serious complications. While a reduction in hospitalization (which incurs more than $3000 in costs for each event on average) is important for reducing healthcare expenditures, a low relapse rate can be expected to substantially improve quality of life for the patient. Poor adherence is hardly unique to the treatment of UC, but the consequences are particularly severe for chronic condition with the potential to progress.
Summary
Adherence to 5-ASA medications for patients with UC in Canada must be improved. In this analysis of a large Canadian database, less than half of patients were still taking the 5-ASA agent associated with the greatest adherence six months after the initial prescription. There are substantial differences between adherence rates for the available 5-ASA agents and appear to be derived from the convenience of the formulation. Patients must be counselled to understand that there are many benefits to remaining on 5-ASA therapy for the treatment of UC that will directly affect their quality of life. Not only will adherence to medication manage symptoms, but it will lower the risks of relapse, hospitalization, surgery and colorectal cancer. These data suggest that new strategies to improve adherence are urgently needed to reduce the morbidity and the costs of UC in Canada.