Gastroenterology
American College of Gastroenterology (ACG) 2012 Annual Scientific Meeting and Postgraduate Course
Suboptimal Adherence to Canadian GERD Guidelines: Opportunity for Improved Symptom Control and Patient Care
Las Vegas – Patients being treated for gastroesophageal reflux disease (GERD) often fail to receive adequate therapy, according to an audit of care by primary care physicians in Canada. Although all of the 500 cases in this series were receiving a proton pump inhibitor (PPI), 92% had persistent symptoms. The fact that 86% were taking a standard dose once-daily suggests published guidelines are not being followed. While the Canadian Association of Gastroenterology (CAG) guidelines recommend a standard PPI dose as initial therapy, they also endorse increasing acid suppression for those whose symptoms are not adequately controlled after a trial of 4 to 8 weeks. The goal of these recommendations is to relieve the large adverse effect that persistent GERD symptoms impose on quality of life. The evidence that physicians are not adhering to guidelines was further reinforced by the overuse of endoscopy in comparison to the CAG guidelines which limit this diagnostic tool for specific indications, such as evaluation of Barrett’s esophagus.
The efficacy and safety of proton pump inhibitor (PPI) therapy in gastroesophageal reflux disease (GERD) is so well established that a symptomatic response is considered evidence of the underlying diagnosis. Despite this efficacy, many patients do not achieve adequate symptom control with a standard initial dose. This was strongly reinforced from a recently conducted primary care chart audit study in which 92% of patients on PPI therapy reported persistent heartburn. In this series of patients all but 14% remained on the starting standard dose of a PPI. This is not consistent with current guidelines which are designed to improve patient care.
Missed Opportunities to Relieve GERD Symptoms
“Determining whether patients achieved adequate control on the initial dose and prescribing greater acid control is outlined in the guidelines.”
“Patients who are not controlled on the standard PPI dose should be offered better 24-hour acid control whether this is accomplished by a sustained-release PPI or by twice-daily PPI dosing. Determining whether patients achieved adequate control on the initial dose and prescribing greater acid control is outlined in the guidelines,” reported Dr. David Armstrong, McMaster University, Hamilton, Ontario, who led this study. At least at the primary care level, “guidelines are not being followed with respect to this escalation of acid suppression. One message from this study is that an important opportunity to relieve GERD symptoms is being missed.”
The primary objective of this study was to document whether primary care physicians are adhering to the published Canadian guidelines for the diagnosis and management of patients with GERD. The Canadian Association of Gastroenterology(CAG) guidelines, for which Dr. Armstrong led the writing committee, cover a broad spectrum of management decisions in 61 consensus statements (Armstrong D et al. Can J Gastroenterol 2005;19:15-35). Each statement is placed in the context of supporting evidence and the degree of consensus among the participating experts, including the statements that address key issues for GERD, including symptom-based diagnosis and management, the role of PPIs as first-line therapy, the need to reassess symptoms 4 to 8 weeks after starting therapy, and the value of increasing acid suppression in those whose symptoms are not controlled with standard dose therapy.
The web-based chart audit program included 500 profiles of patients who were eligible for inclusion if they were taking a PPI for moderate-to-severe symptoms. Most patients had been diagnosed with GERD more than a year before the audit was taken. The average age of those enrolled was 58 years.
While the audit inquired about symptom control rather than other indicators of effectiveness, such as satisfaction with treatment, the lack of adequate control is reinforced by the fact that 30% of patients were taking additional prescription or non-prescription medications to control symptoms of GERD. In the guidelines, stepping up from the standard PPI regimen is the next step when symptoms persist.
The CAG guidelines state that when GERD symptoms persist, treatment needs to step up from the standard PPI regimen to extend acid control, rather than intensify the once-daily dose.
By stepping up, the goal is generally to extend acid control rather than intensify the once-daily dose. Higher, single daily doses usually offer only a marginal added benefit because inadequate acid control is typically due to newly-activating proton pumps. Due to the short half-life of PPIs, inhibition of these newly-activated acid pumps requires reintroduction of active therapy. This is the reason why sustained-release or additional PPI doses are needed when standard doses are inadequate. PPIs act by binding irreversibly to active proton pumps at the time of administration. While this may be sufficient in many individuals, continued acid production by newly-activated pumps may lead to persistent symptoms. This explains why patients with inadequate symptom control often complain of nighttime symptoms. In the current study, half of both men and women complained of persistent nighttime symptoms (Fig. 1).
The reason that poorly-controlled GERD is not addressed with more effective acid control is unclear, but Dr. Marc Bradette, Chief of Service, Hôpital Hôtel-Dieu, Centre Hospitalier Universitaire de Québec, Québec, indicated that it is most likely due to inadequate follow-up after PPIs are prescribed, although lack of awareness about the availability of strategies to improve acid suppression may also play a role.
“I believe physicians do not systematically ask patients if their symptoms are controlled, especially regarding the nighttime symptoms,” observed Dr. Bradette, who was a co-author of this study. “Some physicians may think that increasing acid suppression may not be possible but this is certainly less of an issue than asking their patients if they still have symptoms.”
Although any of the available PPIs typically administered in a once-daily dose can be administered in a twice-daily regimen, the only sustained-release PPI available in Canada is dexlansoprazole. This agent uses a delayed-release technology, which provides a second release of drug and a second peak plasma concentration, thereby binding to newly-activating acid pumps and blocking acid production over a longer proportion of a 24-hour dosing period.
For many patients, the once-daily approach may improve convenience, particularly because PPIs should be administered about a half-hour before meals to maximize the inhibition of food-stimulated proton pump activation. To the degree that twice-daily dosing reduces adherence, a once-daily sustained-release PPI also has the potential to lead to greater efficacy. Reflecting current PPI prescribing patterns, most patients in the chart audit were started on conventional PPIs with low proportions, having been previously exposed to dexlansoprazole (Fig. 2).
However, the reluctance of physicians to increase the dose of PPI therapy to improve symptom control, despite guidelines, does not appear to be restricted to Canada. In a separate study that evaluated a Medicare database in the United States, 96% of 6,568 patients on PPI therapy remained on once-daily dosing. Although this study did not evaluate satisfaction with treatment, previous studies indicate that up to 30% of patients with GERD are not controlled on once-daily therapy. The large adverse effects imposed by uncontrolled GERD symptoms on quality of life are well documented.
In the US study, which was cross-sectional and retrospective, the authors found that those most likely to be prescribed a twice-daily PPI regimen rather than once-daily therapy had been on a PPI longer (≥12 months vs. <6 months), older age, and a higher rate of co-morbidities. According to Dr. Lucinda Chan, PharmD, Touro University College of Pharmacy, Vallejo, California, who was an author on this study, the profile suggests that patients more closely followed for other medical problems may also be more likely to report or be questioned about GERD control, prompting an increased dose when symptoms are inadequately controlled.
It is notable that in the Canadian study, 224 patients, or nearly half of those audited, had previously switched PPI therapy. Although 85 (37.9%) had switched for reasons other than efficacy, such as lack of insurance coverage or adverse events, the majority had switched because of poor symptom control (Fig. 3). There is evidence that patients inadequately responsive to one PPI may respond to another, but the differences in acid control with PPIs administered in standard doses have typically been modest in most controlled studies. In this study, nearly 30% of patients had switched PPI therapy at one point because of poor symptom control even though only about 15% were ultimately given a higher dose as suggested by the guidelines.
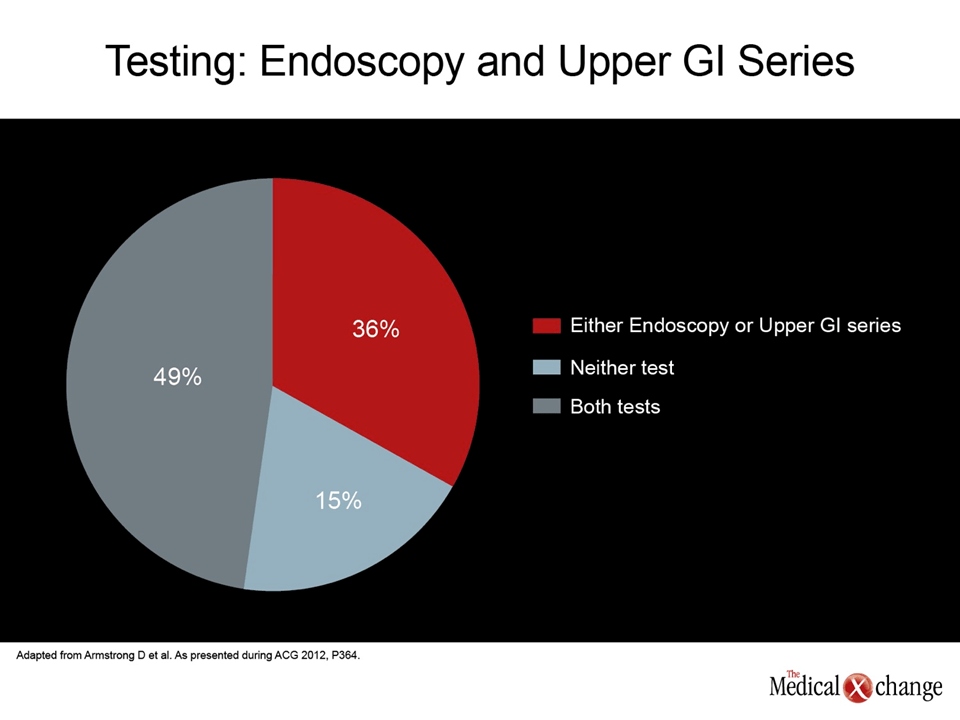
The fact that physicians in Canada are not adhering to CAG guidelines was further advanced by the evaluation of the rate of endoscopic studies in the case audit. The CAG guidelines state that the diagnosis of GERD can be made if the patient has typical symptoms of heartburn or regurgitation; endoscopy is required only to investigate atypical or alarm symptoms and for surveillance of Barrett’s esophagus. In contrast, 85% of the patients audited in this study had been evaluated with an invasive or radiological test (Fig. 4) (2 parts). Furthermore, the proportion that had received endoscopy rose to 100% in those with a history of GERD for more than 5 years.
“The audit suggests that there are substantial opportunities for care optimization,” reported Dr. Armstrong, referring to the gap between the audit’s findings and current recommendations. Suggesting educational initiatives are appropriate, the findings indicate that efforts to bring physicians in line with guidelines would yield better rates of control of GERD and fewer diagnostic studies.
“The audit suggests that there are substantial opportunities for care optimization.”
Conclusion
GERD is a very common condition that can be diagnosed, on the basis of symptoms, without resort to endoscopy or other imaging studies. PPIs are highly effective in the treatment of GERD and well recognized as the first-line therapy for this disease. However, standard doses may not be adequate for a substantial proportion of GERD patients. Once PPIs are initiated, patients should be periodically evaluated for symptom control, including control of nighttime symptoms. This is essential for providing the improvement in quality of life inherent in symptom control. In those with persistent symptoms, escalation of acid control is effective but this is most dependent on extending the duration of acid control over a 24-hour dosing period rather than on an escalation of PPI dose. Both sustained-release and twice-daily PPIs are appropriate strategies to consider. Most GERD patients do not require endoscopy until at least 10 years after the onset of symptoms and every effort should be made to optimize medical therapy for patients with persistent symptoms before considering further investigations.