Respirology
American Thoracic Society (ATS) International Conference 2017
ACTIVATE Trial: Controlling COPD Symptoms to Improve Physical Activity and Change Outcome
Washington, DC – The management of chronic obstructive pulmonary disease (COPD) has transitioned from improving lung function to the broader goal of improving physical capacity, according to a series of studies presented at ATS 2017. By controlling symptoms and improving physical activity, the goal is not just an improvement in quality of life but also an improvement in overall health status. In patients with COPD, comorbidities, such as heart failure and vascular disease, are often the cause of death. Management that results in an improvement in physical activity has been shown to extend survival.
Mortality beyond Lung Disease
In patients with COPD, optimized lung function can only be part of the effort to improve long-term survival, because only about half of deaths are attributed to respiratory failure or other direct consequences of lung impairment. This supports greater emphasis on connecting improved lung function to greater activity levels. Both steps are essential to the effort to help patients with COPD live longer. “If they are sustained, even relatively modest gains in physical activity have the potential to keep COPD patients out of the hospital and living longer,” reported Dr. Thierry Troosters, Department of Rehabilitation Sciences and Respiratory Division, University Hospitals Leuven, Belgium. At this year’s ATS, Dr. Troosters presented results of the ACTIVATE trial, which included change in physical activity as an endpoint. He emphasized that improvement in lung function is not enough for a goal of improved prognosis.
“Modest gains in physical activity have the potential to keep COPD patients out of the hospital and living longer.”
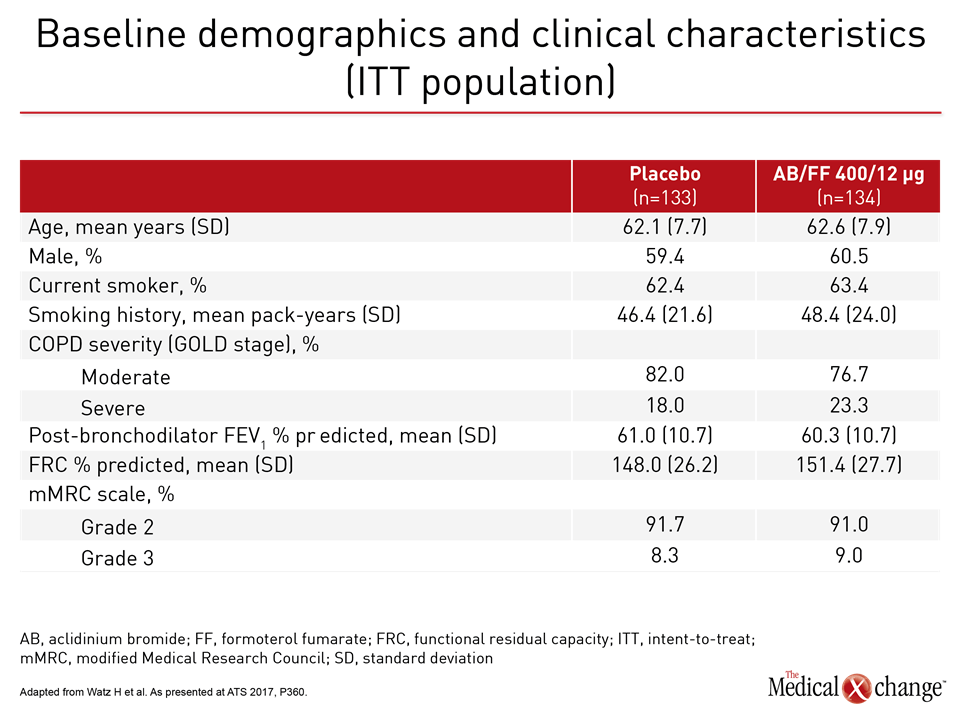
ACTIVATE: Boosting Patient Activity
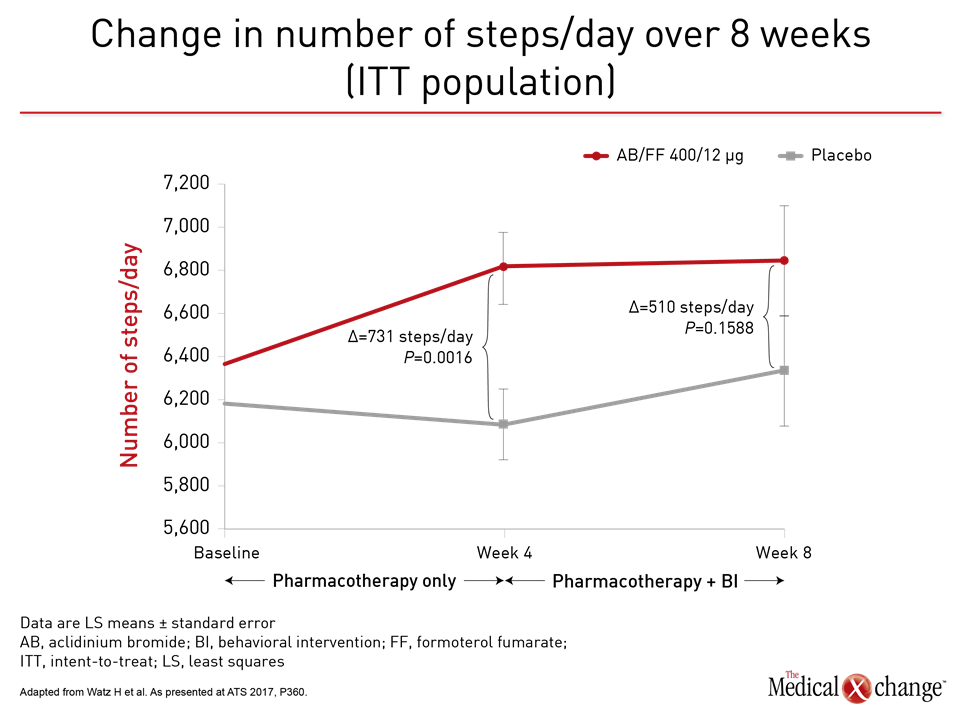
In the phase IV ACTIVATE trial, which is one of the largest trials so far designed to link lung function to exercise capacity, 267 patients with moderate to severe COPD were initially randomized to 400 μg of the long-acting muscarinic antagonist aclidinium and 12 μg of the long-acting beta2-agonist formoterol in a single inhaler or to placebo. After four weeks, patients in both arms initiated an exercise regimen accompanied with an individualized behavioral intervention that encouraged adherence to goals. “The concept was to treat COPD with a potent durable combination therapy in order to optimize lung function and then determine whether we could get patients doing more by treating them effectively,” Dr. Troosters explained. The relatively complex study involved a variety of lung function, exercise capacity, and physical activity endpoints at weeks 4 and 8. Adverse events, including COPD exacerbations, were recorded throughout the 8-week trial.
Helping COPD Patients Do More
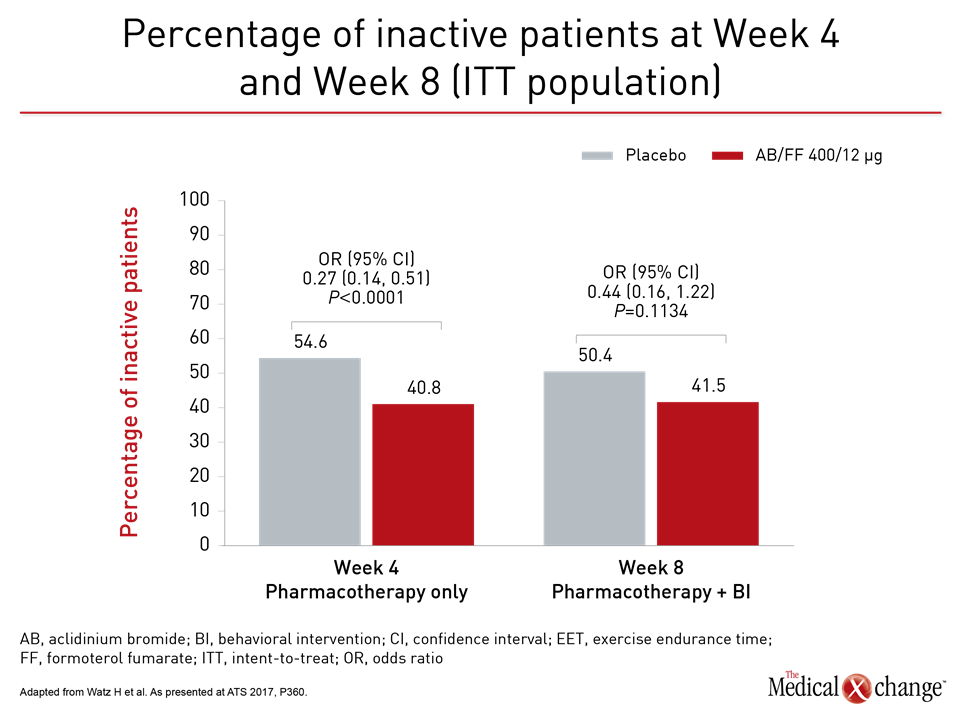
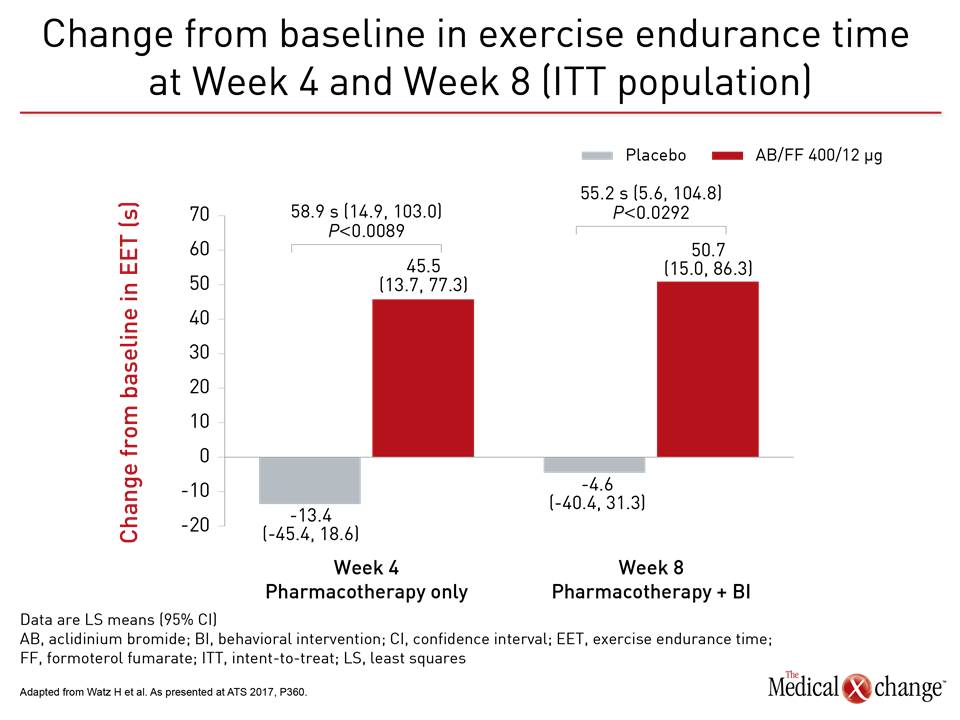
Not surprisingly, there were large relative advantages for those who received aclidinium/formoterol relative to placebo across all measured lung function endpoints at 4 weeks, but the question posed by the study was whether patients with better lung function and symptom control could and would do more. “What the data suggest is that the improvement in lung function and exercise capacity makes it easier and more pleasant to perform the physical activities,” Dr. Troosters explained. “This is important information for getting people off the couch.” One practical measure of increased activity was a mean increase of 731 steps per day at week 4 for those randomized to aclidinium/formoterol relative to placebo (P=0.0016). This clinically significant gain is greater than that recorded in double-blind trials. At week 8, after both groups received the exercise-behavioural intervention, steps per day also improved in the placebo group but the increase on aclidinium/formoterol group was maintained with a mean difference of 510 steps relative to placebo. Consistent with the increased steps per day, which reflects greater activity, was the relative reduction in inactivity for those receiving effective bronchodilation (Fig. 1). At week 4, prior to exercise and behavioral intervention, the proportion of patients on aclidinium/formoterol who remained inactive was lower by a highly statistically significant margin (P<0.0001). At week 8, after the behavioral intervention, the gap was smaller, but Dr. Troosters suggested that the absolute 14% advantage for aclidinium/formoterol over placebo (P=0.1134), is still relevant for long-term prognosis.
Focusing on Long-Term Outcomes
“The earlier in COPD that you improve activity levels, the longer you have an opportunity to make an impact on long-term risks such as cardiovascular events,” said Dr. Troosters, who was also involved in the PHYSACTO trial, which also explored the advantages of combining bronchodilator therapy with specific strategies to promote sustained physical activity. “We are likely to see these strategies reflected in management guidelines.” Others presenting data at ATS 2017 on strategies to sustain physical activity in COPD patients made the same point. One of these, Dr. Janet Larson, Chairman, Department of Health Behavior and Biological Sciences, University of Michigan School of Nursing, Ann Arbor, presented results on a pilot study with an intervention called Active For Life. The pilot study for a larger study being funded by the US National Institutes of Health (NIH) enrolled moderate-to-severe COPD patients who were already on optimized therapy. The program combines education with behavioral and exercise individualized for patient abilities and goals. The program constantly provides reinforcement to keep patients on track. A device worn on the leg measures time upright, relative to sitting or lying down to objectively gauge treatment efficacy.
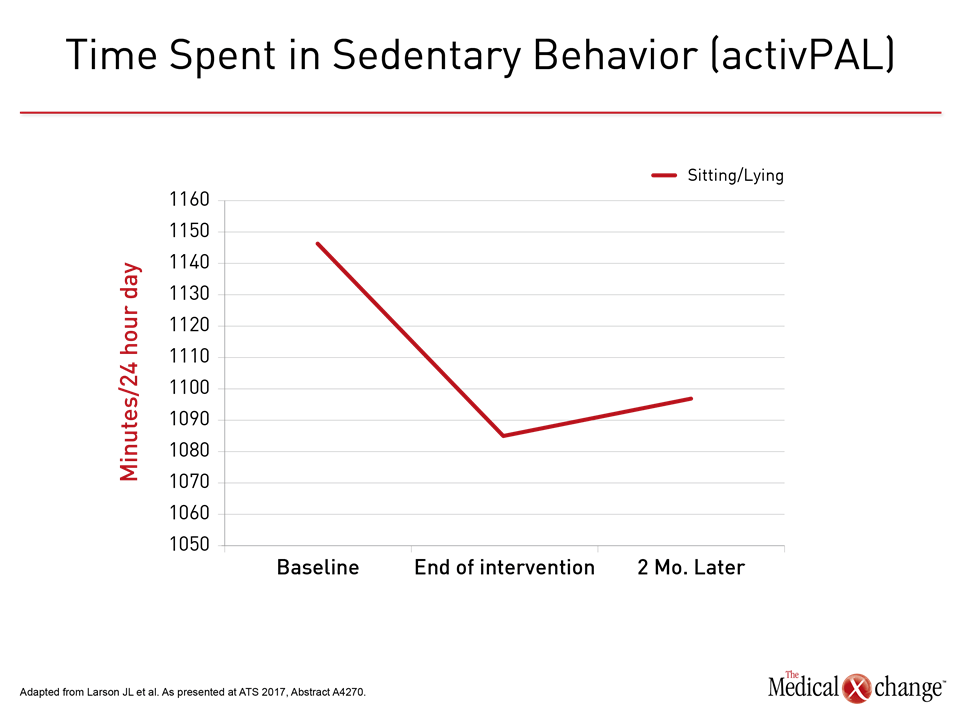
Endpoint: Getting Off the Couch
The study, although small, associated the program with a 60-minute increase in physical activity per day from baseline (P=0.029). Eighty percent of the gain was sustained at 2 months (Fig. 2). “For many patients with COPD, physical activity is overwhelming, so modest and reasonable goals are important to obtain the sustained improvements in activity that will make a difference to long-term outcomes,” Dr. Larson explained. Echoing the remarks by Dr. Troosters, Dr. Larson said, “For many COPD patients, it is very difficult to get off the couch. Yet, this is essential to change their prognosis.”