Expert Review
Management of Hypoactive Sexual Desire Disorder in Women: Awareness & Treatments
Chapter 1: Hypoactive Sexual Desire Disorder
Dr. Marla Shapiro C.M.
MDCM, CCFP. MHSc, FRCPC, FCFP, NCMP
Professor , Family and Community Medicine
University of Toronto, Ontario
Atlanta – Hypoactive Sexual Desire Disorder (HSDD) is a condition that is estimated to affect 7% to 10% of the global population of women. Recently, there has been an evolution in thought with respect to the definition of HSDD and its classification and nomenclature. Recent revisions distinguish HSDD from other disorders of female sexual dysfunction such as female genital arousal disorder (FGAD).
Introduction
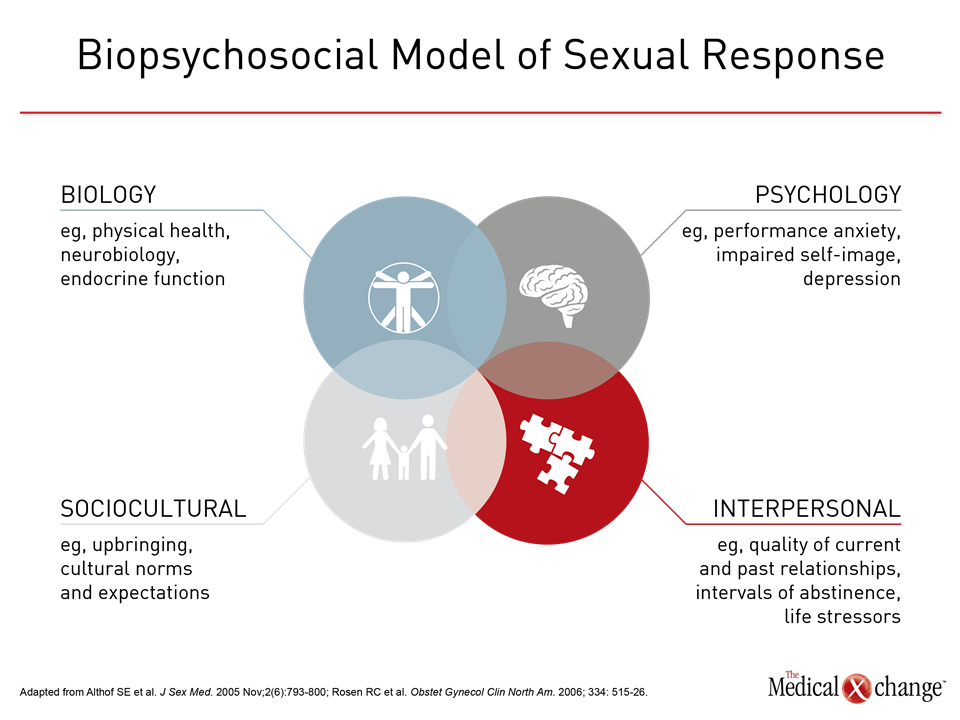
Sexual desire and sexual response are complex, involving biological, psychological, sociocultural, and interpersonal elements (Fig. 1).1 As such, there have been various estimates of the prevalence of hypoactive sexual desire disorder (HSDD). Initial epidemiological research did not necessarily ensure that patients who reported low sexual desire also expressed distress; more recent prevalence figures do reflect the presence of this chief symptom of HSDD. There are several nomenclatures available to describe HSDD, a condition that is estimated to affect about 10% of adult women.2 There has been an evolution in thought with regards to the definition of HSDD. It is now recognized by ISSWSH that HSDD differs from other disorders of female sexual dysfunction such as female genital arousal disorder (FGAD).
Non-ISSWSH Classifications of HSDD
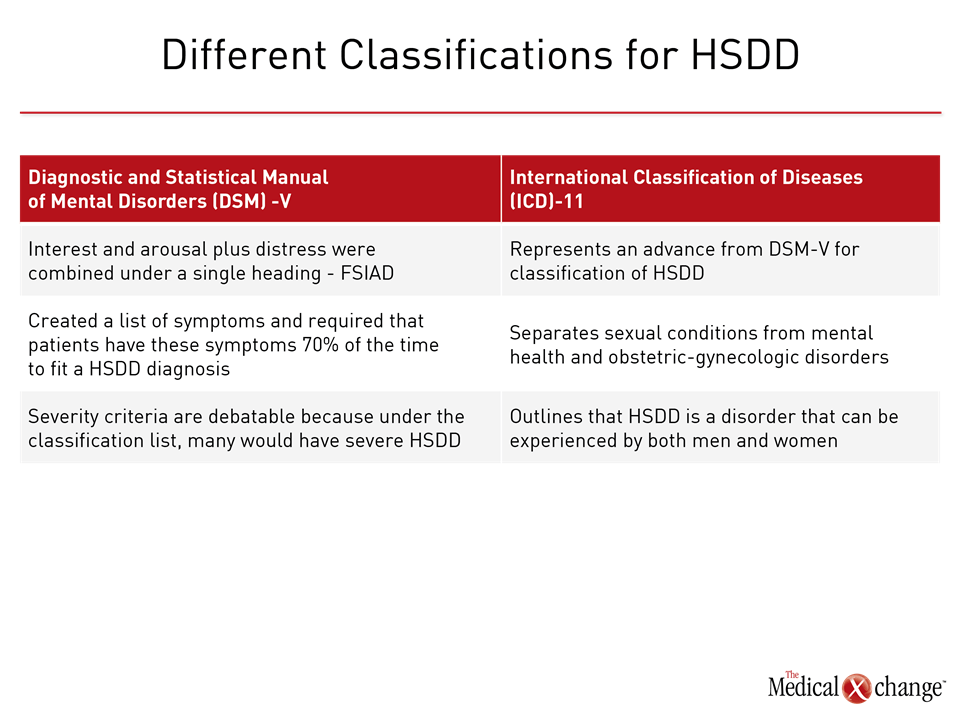
The Diagnostic and Statistical Manual of Mental Disorders (DSM) system, a classification system of the American Psychiatric Association, in its fourth classification system (DSM-IV), provides for broad sexual complaint in specific phases, such as desire or genital arousal, as well as distress not due to any known condition or substance. As an example, a woman who is post-partum and expressing a decreased sexual desire, for example, would not be diagnosed with HSDD. Rather, her decreased desire would be attributed to being post-partum.3 The conditions that were included in this nomenclature are HSDD and female sexual arousal disorder (FSAD). In a subsequent classification system, under the DSM-V, interest and arousal plus distress were combined under a single heading. The DSM-V combined the diagnoses of HSDD and female sexual arousal disorder (FSAD) into female sexual interest/arousal disorder (FSIAD). The DSM-V also created a list of symptoms and required that patients have these symptoms 70% of the time in order to fit a diagnosis of HSDD. These criteria would overlook patients who have more mild or moderate degrees of HSDD, according to Dr. Anita Clayton, Chair, David C. Wilson, Professor, Psychiatry and Neurobehavioral Sciences, University of Virginia Health System, Charlottesville, VA. In terms of diagnosis, “it is less useful,” said Dr. Clayton. “It makes the severity criteria moot because the classification would make everyone have severe HSDD, so it makes the diagnosis very restrictive.” Limitations of the DSM-V provided an impetus for ISSWSH to create an expert consensus panel review to develop a system of diagnostic classification that would distinguish normal sexual variants from sexual function and develop nomenclature on desire disorders, arousal disorders, and orgasm disorders. The emerging nomenclature with International Classification of Diseases (ICD)-11, which clinicians in the US use for billing codes, represents an advance because it separates sexual conditions from mental health and obstetric-gynecologic disorders. “Sexual conditions are in a separate section in ICD-11,” said Dr. Clayton. Of note and different from the DSM-V, ICD-11 outlines that HSDD is a disorder that can be experienced by both men and women (Fig. 2).4
Outcomes from ISSWSH Expert Consensus Panel Review
As mentioned previously, ISSWSH created an expert consensus panel to review existing nomenclatures and to develop a new nomenclature for HSDD, amongst other objectives. “The prior nomenclature was developed by the DSM, which means that it was for the mental health community, and we thought we had to develop something that would work for all of us,” said Sue Goldstein CCRC, AASECT-CSC, IF, of Alvarado Hospital’s Sexual Medicine Program, San Diego, CA.
“The prior nomenclature was developed by the DSM, which means that it was for the mental health community, and we thought we had to develop something that would work for all of us.”
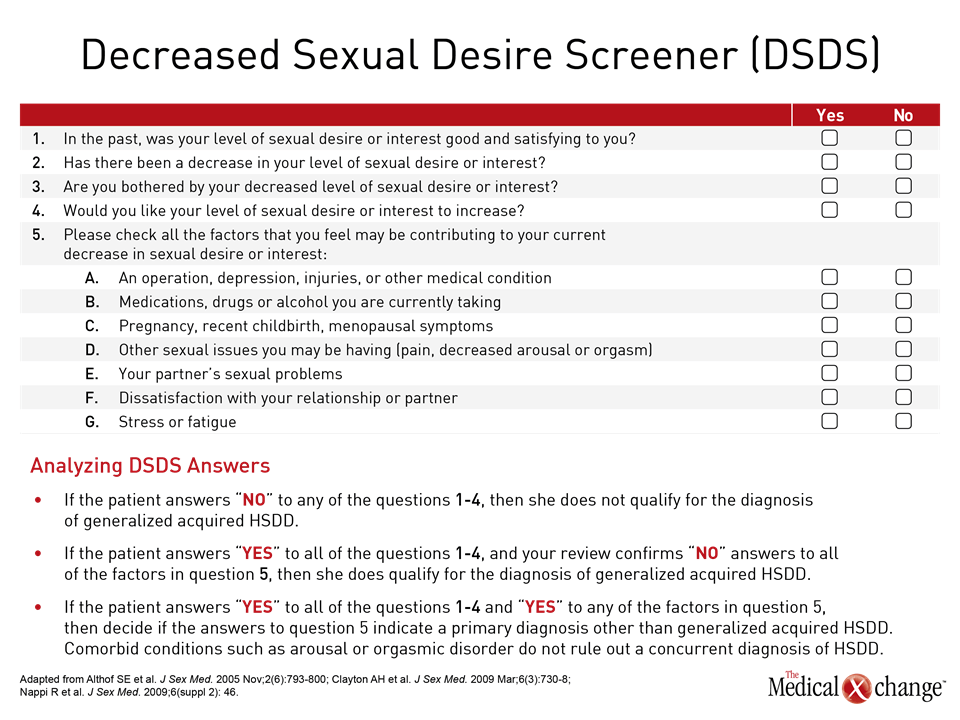
Dr. Sharon Parish, Professor of Medicine, Clinical Psychiatry, Weill Cornell Medicine, NY, noted the fourth International Consultation on Sexual Medicine in 2015, from which a consensus statement aimed at refining the definitions of sexual dysfunctions in women and men emerged. ICSM 4 defined HSDD as “persistent or recurrent deficiency or absence of sexual/erotic thoughts or fantasies and desire for sexual activity.”5 The ISSWSH nomenclature clearly differentiates between HSDD and FSAD, denoting that the former indicates a lack of motivation for sex and lack of desire coupled with distress while FSAD impairs genital response coupled with distress.6 In contrast to HSDD, female genital arousal disorder (FGAD) denotes an inability to develop and maintain genital arousal.6 One of the apparent ways in which HSDD and FGAD differ is in how the diagnosis of each condition is reached. HSDD is arrived at through an interview with the patient and tools like the Decreased Sexual Desire Screener (DSDS), which detects generalized and acquired HSDD in women, can be employed (Fig. 3).7 FGAD is diagnosed through physical examination given questionnaires have not yet been validated for this new diagnosis, noted Dr. Andrew Goldstein, Director of the Centers for Vulvovaginal Disorders in Washington, DC and NY, NY and Clinical Professor at the George Washington University School of Medicine in Washington, DC. As Dr. Clayton noted, an advance in ICD-11 is a separate chapter on sexual health that separates desire and arousal into distinct dysfunctions, according to Dr. Parish. “The separation of the two (arousal and disorder) was based on the clinical principle and similar biologic evidence used by the ICSM and ISSWSH nomenclature processes,” said Dr. Parish, adding that the ICD-11 chapter on sexual health allows HSDD to be applied to either men or women.4
Diagnosing HSDD Using the ISSWSH Nomenclature
The ISSWSH recommends that clinicians pose open-ended questions to arrive at a diagnosis of HSDD. Dr. Clayton stressed that clinicians need not gather intimate details of sexual activity in a patient interview. The PLISSIT technique (Permission, Limited Information, Specific Suggestions, Intensive Therapy) can be used to identify sexual concerns and initiate non-pharmacological management.8 The diagnosis of HSDD is arrived at mainly through clinical presentation; there are no laboratory values that can lead to a diagnosis of HSDD. It is critical for clinicians to take a sexual and reproductive history and assess if there has been sexual trauma, which may be a source of diminished desire. It is also critical to evaluate if decreased desire is specific to the current relationship or if it generalizable to potentially all partners. Similarly, there is a temporal aspect to sexual desire. Diminished desire may be situational and owing to daily life stressors. As an example, it may be that taking a vacation increases desire, said Dr. Clayton.6 Duration of symptoms has become more important to arriving at a diagnosis of HSDD. “The data support having this problem for three months or longer,” said Dr. Clayton. The significance that a patient attaches to sex in her life is also a factor in evaluating the presence of HSDD, according to Dr. Clayton. “You want to know where people prioritize sex in their lives,” said Dr. Clayton. “You want to know where they prioritized sex when they used to have a satisfactory sex life and where the priority for sex is now, that they don’t have a satisfactory sex life.” Loss of desire to initiate sexual activity as well as an avoidant behaviour, such as not going to bed at the same time with a partner on an ongoing basis and/or staying up late to work, is an illustration of behaviour that would be consistent with an HSDD diagnosis, according to Dr. Clayton. Similarly, a woman might avoid kissing her partner as it may signal receptivity to sexual activity. Dr. Parish stressed that sexual desire is not specifically event-related and that fact should be considered in the diagnosis and the management of HSDD.6 Patient Input in an HSDD Diagnosis Indeed, an important criterion for women with acquired HSDD is that they have known a stage in their life where they had sustained sexual desire and are aware they no longer have sustained sexual desire, according to Dr. James G Pfaus, Professor of Psychology, Concordia University, Montreal, Quebec.
“HSDD as a whole should be rated by the person affected as mild, moderate, or severe. Give the person the chance to be part of the diagnosis.”
“By definition, these women have experienced healthy, adequate desire and are distressed to have lost it,” said Dr. Pfaus. “HSDD as a whole should be rated by the person affected as mild, moderate, or severe. Give the person the chance to be part of the diagnosis.”6 The motivations behind sexual desire should be considered, whether sexual desire is a wish to participate in sexual activity with a goal of physical pleasure, emotional intimacy, or other reasons. Desire can be attached to reward and desire can diminish overtime with diminishing sexual reward over time. Ruling Out Other Causes of Low Sexual Desire Citing data from a meta-analysis, Dr. Clayton highlighted the bi-directional relationship that exists between depression and sexual dysfunction where the presence of depression increases the risk of sexual dysfunction and, conversely, the presence of sexual dysfunction greatly increases the risk of depression.9 Taking a detailed sexual history is key in a general assessment of a patient, since past sexual experience can influence a desire for sex. A myriad of other factors can contribute to decreased desire that is causing distress including physiologic co-morbidities like thyroid disease and urinary incontinence and psychiatric conditions like anxiety and depression, as well as the use of medications or substances of abuse.10 Women who have pain disorders would not be regarded as having HSDD. The diminished desire and/or avoidance of sex would be a consequence of the pain experienced during sex, explained Dr. Clayton. Part of the process in arriving at a diagnosis of HSDD in a pre-menopausal woman is ruling out sexual dysfunction in the partner. There can be instances where women report having diminished desire to compensate for sexual dysfunction, such as erectile dysfunction, on the part of her partner. “There is an impact on the woman where she accommodates to that,” explained Dr. Clayton. “She may report it as her own sexual dysfunction.”
Conclusion
According to the ISSWSH expert panel, the recent distinction between HSDD and FGAD as two discrete clinical entities, both of which are diagnoses of female sexual dysfunction, respond to a multi-disciplinary need for practical definitions that will serve various communities in healthcare including clinicians, researchers, and regulatory agencies. “This definition (of FGAD) completely excludes the central issue such as subjective arousal that was controversial and convoluted in prior definitions of FSAD. In so doing, it strengthens both the new definition of FGAD as well as the definition of HSDD,” said Dr. Goldstein.
References
1. Althof SE, Leiblum SR, Chevret-Measson M, et al. Psychological and interpersonal dimension of sexual function and dysfunction. J Sex Med. 2005 Nov;2(6):793-800 2. Goldstein I, Kim NN, Clayton AH, et al. Hypoactive Sexual Desire Disorder: International Society for the Study of Women’s Sexual Health (ISSWSH) Expert Consensus Panel Review. Mayo Clin Proc. 2017 Jan;92(1):114-128 3. DeJudicibus MA, McCabe MP. Psychological factors and the sexuality of pregnant and postpartum women. The Journal of Sex Research. 2002 May;39(2):94-103. 4. Reed GM, Drescher J, Krueger RB, et al. World Psychiatry. 2016 Oct;15(3):205-221 5. McCabe MP, Sharlip ID, Atalla E, et al. Definitions of Sexual Dysfunctions in Women and Men: A Consensus Statement from the Fourth International Consultation on Sexual Medicine 2015. J Sex Med. 2016 Feb;13(2):135-43 6. Parish SJ, Goldstein AT, Goldstein SW, et al. Toward a More Evidence-Based Nosology and Nomenclature for Female Sexual Dysfunctions-Part II. J Sex Med. 2016 Dec;13(12)1888-1906 7. Clayton AH, Goldfischer ER, Goldstein I, Derogatis L, Lewis-D’Agostino DJ, Pyke R. Validation of the decreased sexual desire screener (DSDS) J Sex Med. 2009 Mar;6(3):730-8 8. Frank JE, Mistretta P, Will J. Diagnosis and treatment of female sexual dysfunction. Am Fam Physician. 2008 Mar 1;77(5):635-42
Chapter 1: Hypoactive Sexual Desire Disorder
Atlanta – Hypoactive Sexual Desire Disorder (HSDD) is a condition that is estimated to affect 7% to 10% of the global population of women. Recently, there has been an evolution in thought with respect to the definition of HSDD and its classification and nomenclature. Recent revisions distinguish HSDD from other disorders of female sexual dysfunction such as female genital arousal disorder (FGAD).
Show review