Ophthalmology
American Academy of Ophthalmology (AAO) 2018
Treatment Options on the Horizon for Glaucoma Management
Chicago – Adherence to medical therapy among glaucoma patients is less than optimal. To respond to this challenge, investigators are exploring alternative strategies for delivering medical therapies. To make these sustained-release platforms viable, at-home intraocular pressure (IOP) monitoring will likely become an element in overall glaucoma management.
Addressing Poor Patient Adherence to Therapy
Statistics from one US study found close to one half of patients who had filled a glaucoma prescription discontinued medical therapy within six months and just slightly more than one-third (37%) had refilled their initial medication at three years after the first prescription was dispensed (Nordstrom BL et al. Am J Ophthalmol. 2005;140:598-606). Of note, patients with diagnosed open angle glaucoma were more likely to adhere to treatment than those with suspected glaucoma. Further, although the study showed differences in adherence among the four drug classes tested, these results indicate that there is indeed room for improvement.
At this year’s American Academy of Ophthalmology (AAO) scientific meeting during the Glaucoma Subspecialty Day sessions, Dr. James D. Brandt, Professor of Ophthalmology and Vision Science and the Director of the Glaucoma Service at the University of California, Davis, California, presented some examples of devices under study that may offer alternative options in controlling IOP.
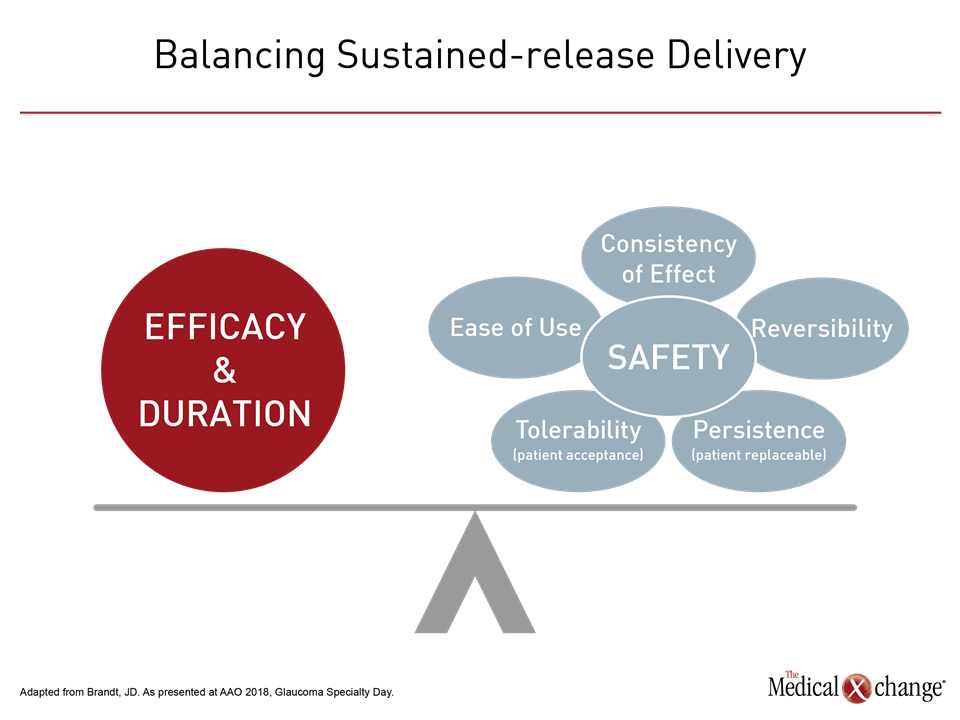
“We have a significant treatment paradox,” said Dr. Brandt. “We have highly-effective treatments that work [eye drops], but we know as many as 50% of our patients do not take their drops. Also, we are very poor at identifying patients who are compliant and those who are not. Sustained-release delivery will help us address this challenge. It has the potential for long-term IOP control without daily dosing” (Fig. 1).
IOP Home Monitoring
Home monitoring of IOP will be a necessary component in glaucoma care should sustained-release therapies become available, according to Dr. Brandt. “An integral part of the acceptance of sustained-release [therapies] is going to be home tonometry,” he said, noting symptoms do not occur that indicate to patients that they are experiencing IOP elevation and require treatment.
“Right now, we just get snapshots of IOP in the clinic,” according to Dr. Patrick Gooi, Glaucoma Subsection Lead, University of Calgary, Alberta. “IOP fluctuates over the course of 24 hours. Data management with home tonometry will be important so that we can get reliable data and transfer the data in a secure and meaningful way to physicians.”
“If you see that IOP is fluctuating more than the clinical visits suggest, that may lead toward escalating therapy, with drops, laser, or surgery.”
The data that home tonometry technologies would generate could inform therapeutic choices. “If you see that IOP is fluctuating more than the clinical visits suggest, that may lead toward escalating therapy, with drops, laser, or surgery,” said Dr. Gooi.
Conclusion
More treatment options and improved IOP monitoring may allow clinicians to make more informed, individualized management plans for glaucoma patients.