Expert Review
Unmet Needs in PPI Therapy for GERD
Chapter 2: Nighttime GERD – Implications for Clinical Practice
Marc Bradette, MD, FRCP
Pavillon Hôtel-Dieu de Québec, Centre Hospitalier Universitaire de Québec
Québec, QC
Of patients who report at least once-weekly episodes of heartburn, most also report nighttime symptoms. Although both the daytime and nighttime subtypes of gastroesophageal reflux disease (GERD) are produced when acidic gastric contents reflux into the lower esophagus, nighttime reflux has the potential to be a more severe form. Probably due to the loss of gravity that increases acid dwell time in the esophagus in the supine position, nocturnal reflux is associated with a higher risk of esophagitis and its long-term complications. Effective treatment of daytime reflux is not necessarily effective for nighttime episodes for a variety of reasons, including diminishing pharmacologic effect from proton pump inhibitors (PPIs) that are typically taken once daily in the morning. In many patient groups, such as those with sleep apnea, nocturnal GERD can contribute substantially to complications such as daytime fatigue. Due to its distinct features and risks, nocturnal GERD should be addressed specifically with the goal of complete symptom control.
Definition and Epidemiology
Large surveys of patients with GERD suggest that about 80% of patients with daytime GERD also have nighttime symptoms.
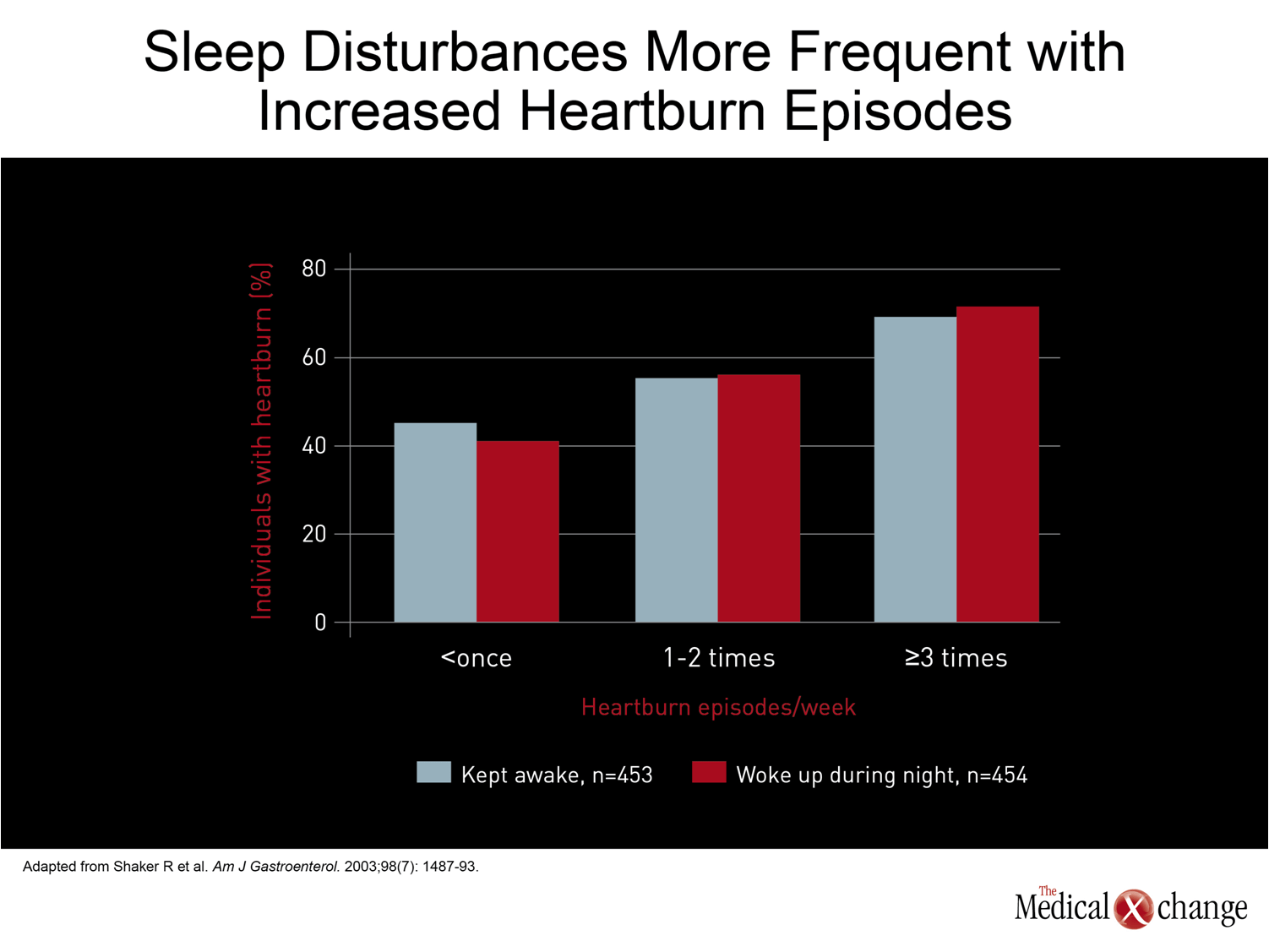
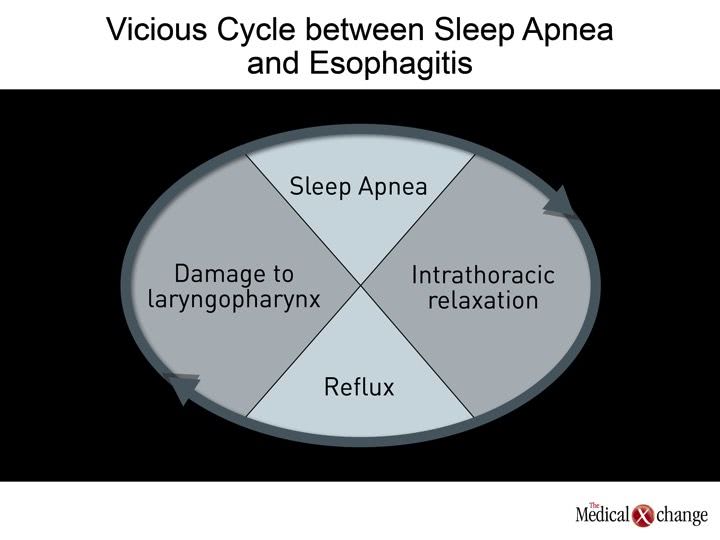
By the most commonly-used definition, patients have nocturnal gastroesophageal reflux disease (GERD) when heartburn or other symptoms adversely affect sleep quality.(1)This can refer to difficulty getting to sleep, mid-sleep awakenings, or a sense of next-day fatigue. Large surveys of patients with GERD suggest that about 80% of patients with daytime GERD also have nighttime symptoms.(2-3)In one survey of patients with GERD, 47% reported that symptoms sometimes or frequently woke them in the middle of the night.(4)In another, 63% reported that GERD symptoms adversely affected the quality of their sleep, and 40% reported that nocturnal heartburn affected their ability to function the next day.(5)The likelihood of nocturnal symptoms increased with the frequency of daytime symptoms (Fig. 1). Although most surveys have focused on heartburn as the source of sleep disturbances, other GERD symptoms, such as regurgitation, may make important contributions. In particular, there is a strong association between GERD and sleep apnea.(6-7)It has been hypothesized that this association is the result of a vicious cycle when gastric contents reach the upper airways to cause inflammatory damage.(8-9)According to this theory, sleep apnea which is induced or exacerbated by this damage, reduces intrathoracic pressure to increase reflux events, thereby increasing the risk for further reflux, further inflammation, and persistent apnea risk . Other extraesophageal symptoms of GERD, such as chronic cough, may also be involved in clinically significant disturbances of sleep or sleep quality.(10)
Impact of Nocturnal GERD on Quality of Life
There is substantial evidence that GERD episodes at night are more serious than GERD events during the day. Nocturnal GERD is associated with a greater risk of esophagitis and severe forms of esophagitis, a greater risk of Barrett’s esophagus.
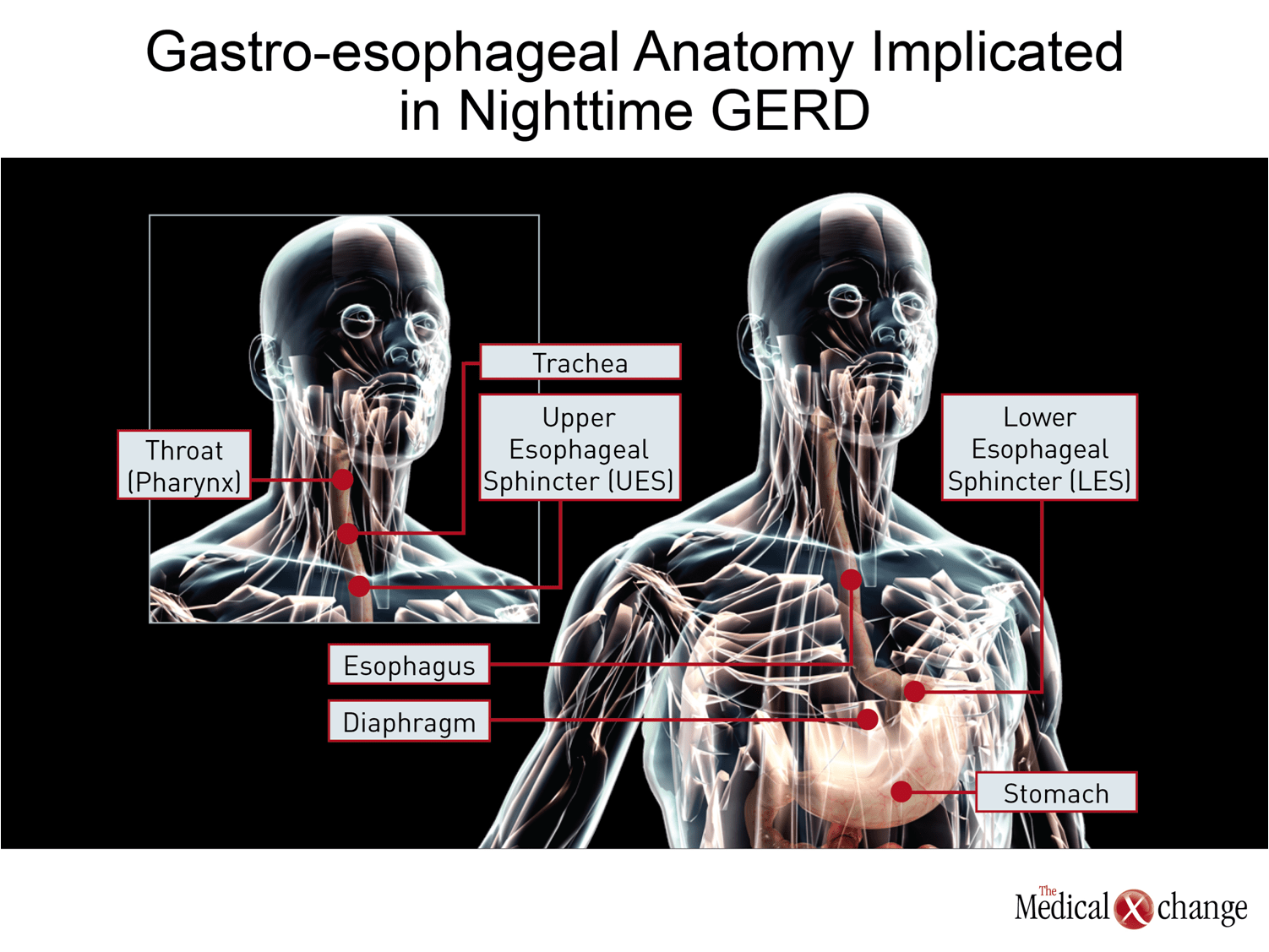
The adverse impact of nocturnal GERD on quality of life has been demonstrated repeatedly,(11-12)but there is also substantial evidence that GERD episodes at night are more serious than GERD events during the day. Nocturnal GERD is associated with a greater risk of esophagitis and severe forms of esophagitis,(13)including a greater risk of Barrett’s esophagus.(14)The likely explanation is that the events occurring in the supine position produce slower clearance of the reflux so that longer acid contact increases the risk of damage.(15-16)The reduction in gravitational forces inherent in the supine position may also increase the likelihood that reflux will extend higher into the esophagus, reaching the airways to exacerbate sleep apnea and other extraesophageal manifestations.(17) (Fig. 2) Nighttime symptoms have also been associated with diminishing next-day work productivity.(18)In a study which compared 476 individuals with GERD who had nocturnal symptoms to 526 individuals with GERD but no nocturnal symptoms and 513 controls, the reduction in work productivity and GERD-related work loss were highly significant (P<0.0001) relative to either the GERD group without nocturnal symptoms or controls.(19)(Fig. 3)
Pathophysiology
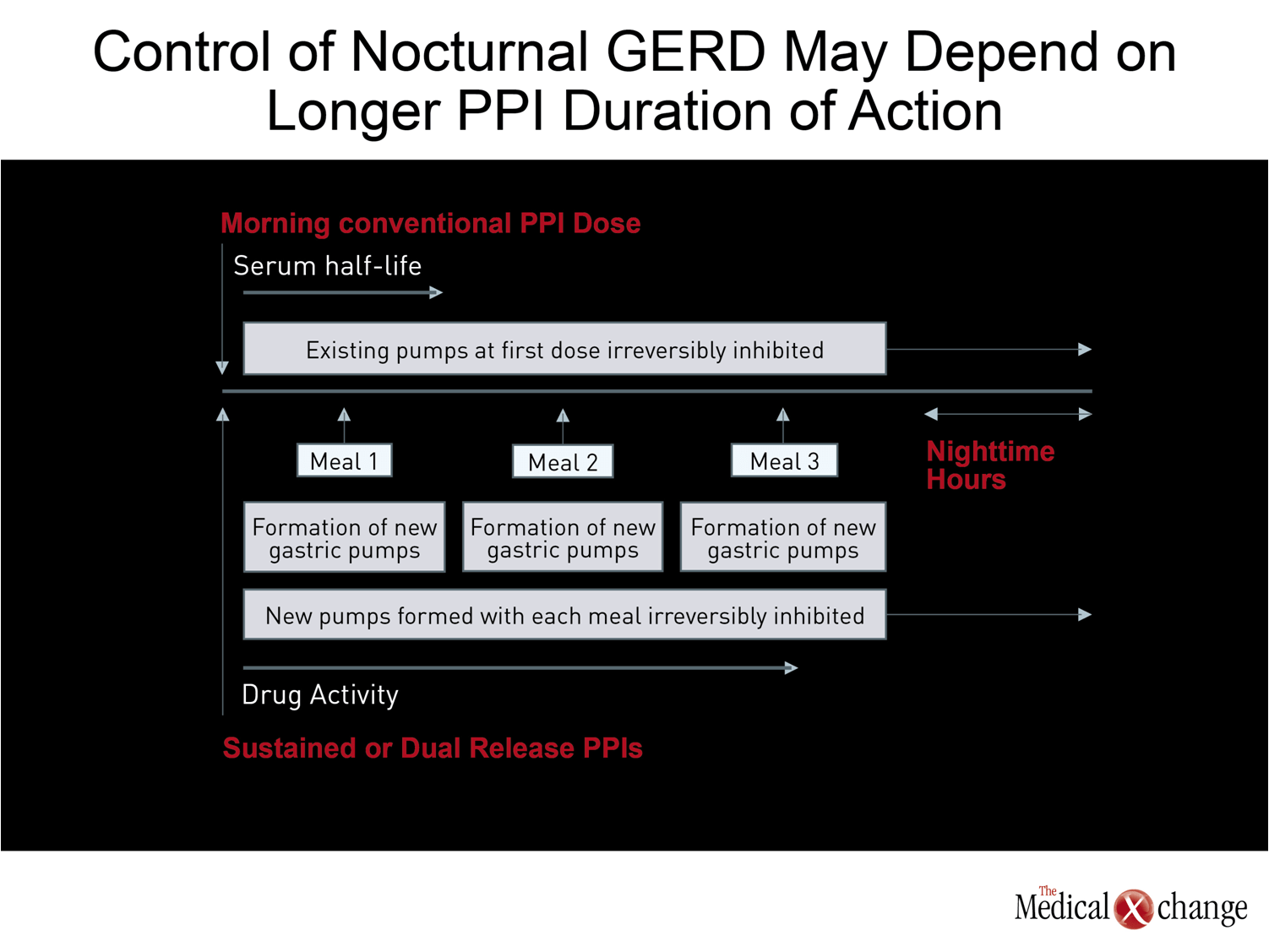
Although the vast majority of patients with daytime GERD also have clinically significant nocturnal symptoms, risk factors for nocturnal symptoms may differ. In relatively large surveys, nocturnal GERD risk factors have included more daily symptoms of heartburn, severe daytime symptoms, predominant symptom of regurgitation, long duration of GERD symptoms, and higher body mass (BMI).(20-21)Sleep apnea, as previously mentioned, is also associated with nocturnal GERD, and there is a correlation between greater severity of apnea and greater likelihood of GERD.(6)While the correlation between severe or frequent symptoms of daytime heartburn symptoms may relate to a weaker barrier to reflux episodes, such as hiatal hernia,(21)the increase in BMI is likely to not only increase the risk of GERD but the proximal extent of the rise in gastric contents.(22) The basic mechanism of GERD, which includes a greater or more prolonged acid exposure in the lower esophagus after otherwise normal transient lower esophageal sphincter relaxations (TLESR),(23)is likely to be similar in daytime and nighttime GERD, but the precipitating factors may vary. For example, late night meals have been shown to be a risk factor for nocturnal GERD, (24)and agents that increase muscle relaxation, such as benzodiazepines, may also have a more deleterious effect at night than in the day when patients are no longer upright.(21) Impaired barrier function due to a hiatal hernia or other cause may be important to nocturnal GERD in some individuals, but there is some evidence TLESRs are similar in patients with or without GERD and that the difference in risk is mediated by the greater acid content of the reflux, the slower clearance of the acid, or both.(23, 25)This reinforces the importance of anti-secretory therapy to lower gastric acid levels, a step that may be poorly suited to once-daily proton pump inhibitor (PPI) therapy taken in the morning. PPIs irreversibly bind to meal-stimulated proton-pumps, which is the final step for gastric acid secretion, but have a relatively short half-life in the serum.(26)Consequently when new proton pumps are formed with meals later in the day, gastric acid suppression diminishes. This may explain why nocturnal GERD is often more difficult to control and is more likely to produce severe esophagitis.(13)
Treatment
Effective acid control is associated with a reduction in nocturnal GERD, including sleep disturbances,(27)but once-daily PPIs are unable to control nocturnal GERD consistently.(28)This has led to a variety of strategies to improve outcome, including twice-daily PPI therapy,(29)once daily PPI therapy combined with an H2-receptor antagonist at night,(30)and sustained-release or dual-release PPIs.(31-32)Although twice-daily PPIs are effective and are likely to be superior to the combination of a PPI and an H2-receptor antagonist, which would provide weaker acid control at night, this approach is burdened by a more demanding regimen that might diminish compliance. (Fig. 4)
The potential advantages of a sustained- or dual-release PPI for the treatment of nocturnal GERD are substantial based on the pathophysiology of GERD and the pharmacokinetics of antisecretory agents.
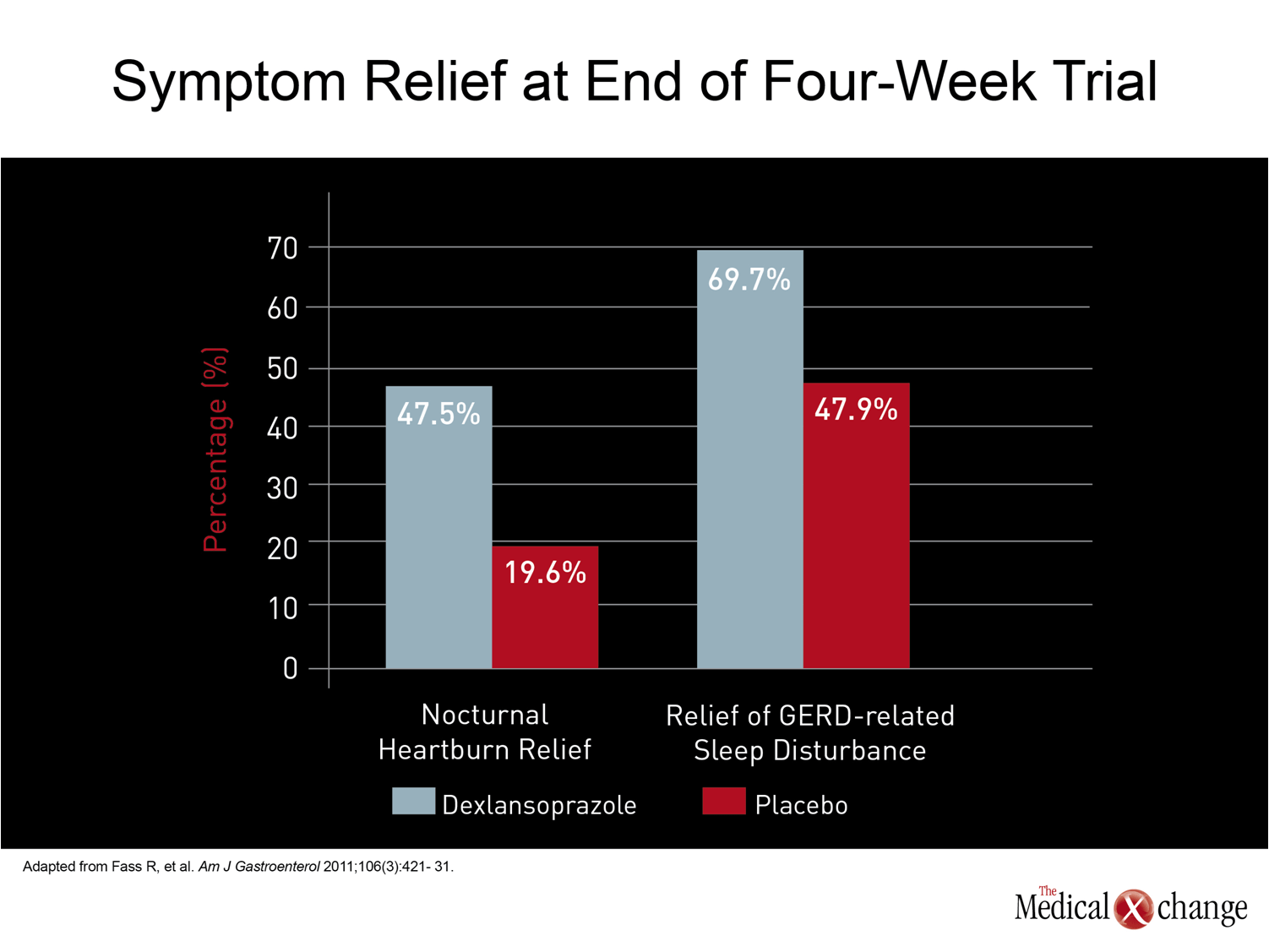
The potential advantages of a sustained- or dual-release PPI for the treatment of nocturnal GERD are substantial based on the pathophysiology of GERD and the pharmacokinetics of antisecretory agents. In a study that compared a sustained-release once-daily dose of 50 mg rabeprazole to a conventional dose of 40 mg once daily esomeprazole, the esophagitis healing rates were slightly greater at 8 weeks for Los Angeles (LA) grade C esophagitis with rabeprazole as compared with esomeprazole (80% vs. 75%), but the symptom relief was comparable (48.3% vs. 48.2%).(33)However, this study did not look at nocturnal symptoms specifically. In contrast, a study of dexlansoprazole modified release (MR), which employs a dual-release technology to separate peak plasma levels, that was conducted specifically in individuals with nocturnal GERD did demonstrate a highly significant reduction in sleep-related symptoms as well as an improvement in work productivity.(32)In this 305-patient trial, relief of sleep disturbances was 69.7% and 47.9% (P<0.001) in placebo in the two study groups, favouring dexlansoprazole. Other strategies can be helpful alone or in combination with acid control for reducing nocturnal GERD and its adverse effects on sleep. Avoiding late evening meals is one reasonable approach, while elevating the head of the bed has a documented benefit on symptom improvement.(1)These mechanical approaches are important, but acid control has been fundamental to the treatment of GERD in both its daytime and nighttime manifestations. Surgical control of fundoplication has been specifically associated with improvement in sleep disturbances due to GERD,(34)but other methods of acid control if effective in the evening hours would be expected to provide meaningful clinical benefit. (Fig. 5)
Conclusion
Nocturnal GERD is an extremely common disorder that deserves specific attention because of its important role in diminishing quality of life as well as the threat it poses to development of esophagitis and its complications, including Barrett’s esophagus and esophageal adenocarcinoma. It cannot be assumed that treatments effective for control of daytime GERD symptoms will be effective in the evening for several reasons, particularly the physiology of meal-stimulated acid pump development. Patients treated for GERD should be asked specifically about nighttime symptom control. Adjustments in treatment, including use of longer-acting agents, may be appropriate if there is a presence of nocturnal GERD. Controlling nocturnal GERD presents a major opportunity to improve patient wellbeing.
References
1. Gerson LB, Fass R. A systematic review of the definitions, prevalence, and response to treatment of nocturnal gastroesophageal reflux disease. Clin Gastroenterol Hepatol 2009;7(4):372-8; quiz 67. 2. Farup C, Kleinman L, Sloan S, et al. The impact of nocturnal symptoms associated with gastroesophageal reflux disease on health-related quality of life. Arch Intern Med 2001;161(1):45-52. 3. Chand N, Johnson DA, Tabangin M, Ware JC. Sleep dysfunction in patients with gastro-oesophageal reflux disease: prevalence and response to GERD therapy, a pilot study. Aliment Pharmacol Ther 2004;20(9):969-74. 4. Locke GR, 3rd, Talley NJ, Fett SL, Zinsmeister AR, Melton LJ, 3rd. Prevalence and clinical spectrum of gastroesophageal reflux: a population-based study in Olmsted County, Minnesota. Gastroenterology 1997;112(5):1448-56. 5. Shaker R, Castell DO, Schoenfeld PS, Spechler SJ. Nighttime heartburn is an under-appreciated clinical problem that impacts sleep and daytime function: the results of a Gallup survey conducted on behalf of the American Gastroenterological Association. Am J Gastroenterol 2003;98(7):1487-93. 6. Shepherd KL, James AL, Musk AW, Hunter ML, Hillman DR, Eastwood PR. Gastro-oesophageal reflux symptoms are related to the presence and severity of obstructive sleep apnoea. J Sleep Res 2011;20(1 Pt 2):241-9. 7. Sabate JM, Jouet P, Merrouche M, et al. Gastroesophageal reflux in patients with morbid obesity: a role of obstructive sleep apnea syndrome? Obes Surg 2008;18(11):1479-84. 8. Morse CA, Quan SF, Mays MZ, Green C, Stephen G, Fass R. Is there a relationship between obstructive sleep apnea and gastroesophageal reflux disease? Clin Gastroenterol Hepatol 2004;2(9):761-8. 9. Kuribayashi S, Kusano M, Kawamura O, et al. Mechanism of gastroesophageal reflux in patients with obstructive sleep apnea syndrome. Neurogastroenterol Motil 2010;22(6):611-e172. 10. Birring SS. New concepts in the management of chronic cough. Pulm Pharmacol Ther 2011;24(3):334-8. 11. Guda N, Partington S, Vakil N. Symptomatic gastro-oesophageal reflux, arousals and sleep quality in patients undergoing polysomnography for possible obstructive sleep apnoea. Aliment Pharmacol Ther 2004;20(10):1153-9. 12. Orr WC, Heading R, Johnson LF, Kryger M. Review article: sleep and its relationship to gastro-oesophageal reflux. Aliment Pharmacol Ther 2004;20 Suppl 9:39-46. 13. Adachi K, Fujishiro H, Katsube T, et al. Predominant nocturnal acid reflux in patients with Los Angeles grade C and D reflux esophagitis. J Gastroenterol Hepatol 2001;16(11):1191-6. 14. Orr WC, Lackey C, Robinson MG, Johnson LF, Welsh JD. Esophageal acid clearance during sleep in patients with Barrett’s esophagus. Dig Dis Sci 1988;33(6):654-9. 15. Orr WC, Allen ML, Robinson M. The pattern of nocturnal and diurnal esophageal acid exposure in the pathogenesis of erosive mucosal damage. Am J Gastroenterol 1994;89(4):509-12. 16. Helm JF, Dodds WJ, Pelc LR, Palmer DW, Hogan WJ, Teeter BC. Effect of esophageal emptying and saliva on clearance of acid from the esophagus. N Engl J Med 1984;310(5):284-8. 17. Jacob P, Kahrilas PJ, Herzon G. Proximal esophageal pH-metry in patients with ‘reflux laryngitis’. Gastroenterology 1991;100(2):305-10. 18. Gross M, Beckenbauer U, Burkowitz J, Walther H, Brueggenjuergen B. Impact of gastro-oesophageal reflux disease on work productivity despite therapy with proton pump inhibitors in Germany. Eur J Med Res 2010;15(3):124-30. 19. Dubois RW, Aguilar D, Fass R, et al. Consequences of frequent nocturnal gastro-oesophageal reflux disease among employed adults: symptom severity, quality of life and work productivity. Aliment Pharmacol Ther 2007;25(4):487-500. 20. Gaddam S, Maddur P, Wani S, et al. Risk Factors for Nocturnal Reflux in a Large GERD Cohort. J Clin Gastroenterol 2011. 21. Fass R, Quan SF, O’Connor GT, Ervin A, Iber C. Predictors of heartburn during sleep in a large prospective cohort study. Chest 2005;127(5):1658-66. 22. Blondeau K, Boecxstaens V, Van Oudenhove L, Farre R, Boeckxstaens G, Tack J. Increasing body weight enhances prevalence and proximal extent of reflux in GERD patients ‘on’ and ‘off’ PPI therapy. Neurogastroenterol Motil 2011. 23. Iwakiri K, Kawami N, Sano H, et al. Mechanisms of excessive esophageal acid exposure in patients with reflux esophagitis. Dig Dis Sci 2009;54(8):1686-92. 24. Piesman M, Hwang I, Maydonovitch C, Wong RK. Nocturnal reflux episodes following the administration of a standardized meal. Does timing matter? Am J Gastroenterol 2007;102(10):2128-34. 25. Hershcovici T, Mashimo H, Fass R. The lower esophageal sphincter. Neurogastroenterol Motil 2011. 26. Sachs G, Shin JM, Hunt R. Novel approaches to inhibition of gastric acid secretion. Curr Gastroenterol Rep 2010;12(6):437-47. 27. Dimarino Jr AJ, Banwait KS, Eschinger E, et al. The effect of gastro-oesophageal reflux and omeprazole on key sleep parameters. Aliment Pharmacol Ther 2005;22(4):325-9. 28. Johnson DA, Katz PO. Nocturnal gastroesophageal reflux disease: issues, implications, and management strategies. Rev Gastroenterol Disord 2008;8(2):98-108. 29. Orr WC, Craddock A, Goodrich S. Acidic and non-acidic reflux during sleep under conditions of powerful acid suppression. Chest 2007;131(2):460-5. 30. Mainie I, Tutuian R, Castell DO. Addition of a H2 receptor antagonist to PPI improves acid control and decreases nocturnal acid breakthrough. J Clin Gastroenterol 2008;42(6):676-9. 31. Howden CW, Ballard ED, Koch FK, Gautille TC, Bagin RG. Control of 24-hour intragastric acidity with morning dosing of immediate-release and delayed-release proton pump inhibitors in patients with GERD. J Clin Gastroenterol 2009;43(4):323-6. 32. Fass R, Johnson DA, Orr WC, et al. The effect of dexlansoprazole MR on nocturnal heartburn and GERD-related sleep disturbances in patients with symptomatic GERD. Am J Gastroenterol 2011;106(3):421-31. 33. Laine L, Katz PO, Johnson DA, et al. Randomised clinical trial: a novel rabeprazole extended release 50 mg formulation vs. esomeprazole 40 mg in healing of moderate-to-severe erosive oesophagitis – the results of two double-blind studies. Aliment Pharmacol Ther 2011;33(2):203-12. 34. Cohen JA, Arain A, Harris PA, et al. Surgical trial investigating nocturnal gastroesophageal reflux and sleep (STINGERS). Surg Endosc 2003;17(3):394-400.
Chapter 2: Nighttime GERD – Implications for Clinical Practice
Of patients who report at least once-weekly episodes of heartburn, most also report nighttime symptoms. Although both the daytime and nighttime subtypes of gastroesophageal reflux disease (GERD) are produced when acidic gastric contents reflux into the lower esophagus, nighttime reflux has the potential to be a more severe form. Probably due to the loss of gravity that increases acid dwell time in the esophagus in the supine position, nocturnal reflux is associated with a higher risk of esophagitis and its long-term complications. Effective treatment of daytime reflux is not necessarily effective for nighttime episodes for a variety of reasons, including diminishing pharmacologic effect from proton pump inhibitors (PPIs) that are typically taken once daily in the morning. In many patient groups, such as those with sleep apnea, nocturnal GERD can contribute substantially to complications such as daytime fatigue. Due to its distinct features and risks, nocturnal GERD should be addressed specifically with the goal of complete symptom control.
Show review